 By Dr. Amanda Craig, PhD, LMFT If you are one of over 14 million Americans affected by a Major Depressive Disorder, you may know firsthand about the debilitating effects of this condition that can leave us feeling incapacitated, hopeless and ashamed. However, if you are a man living with depression, you may be struggling with symptoms without realizing what they mean and without getting treatment. It is a common misnomer that men are less susceptible to depression than women. The reality is that men and women experience depression at roughly the same rate when measured by a gender inclusive depression scale, but their symptoms may be different. Women are also much more likely to seek treatment. This gender-based difference in symptoms can prevent men from recognizing and acknowledging their depression, while gender-stereotyped attitudes about coping deter men from seeking help. Perhaps that’s why the suicide rate among American men is four times higher than among women. Men are four times as likely to commit suicide as women. White middle-aged men are at the highest risk of suicide.Signs of depression in men: Societal norms make it difficult for men to allow themselves the vulnerability to express sadness or weakness. Whereas women are more likely to present with “classic” symptoms like sadness, men are likely to display more socially acceptable “masculine” emotions of anger, aggressiveness, or other symptoms which are not commonly associated with depression. Strong emotions such as anger create the illusion of power and control, but also mask the feelings of defeat, failure, and inadequacy. Although individual experiences may differ, some common depression symptoms among men should be a cause for concern when experienced for longer than two weeks. Fewer signs may suggest a milder depression while more symptoms indicate more severe depression. These include: o Anger, irritability, or aggressiveness o Anxiousness, restlessness, feeling “on edge.” o Feeling sad, empty, or hopeless o Appetite and weight change o Feeling extremely tired or low energy o Difficulty sleeping o Psychomotor agitation or being slowed down as seen by others o Diminished interest in work, family, and activities you once enjoyed o Poor concentration, difficulty remembering things or making decisions o Low self-esteem or self-worth or inappropriate guilt o Suicidal thoughts or plans Physical symptoms of depression may include: o Backaches, headaches, and other body aches o Heartburn and other digestive problems o Decreased sexual desire and performance o High blood pressure (this is very common) Common behaviors related to depression include: o Spending more time at work o Watching excessive sports o Extramarital affairs o Alcohol or drug abuse o Violent or abusive behaviors o Irritability or inappropriate/disproportionate anger o Risky behaviors and excessive risk-taking However, because men may be reluctant to share their struggles, some will internalize their feelings and become withdrawn and aloof. Instead of acting out in aggressive ways they may isolate from family members, display a delay in responding to questions and conversations, and miss important deadlines.
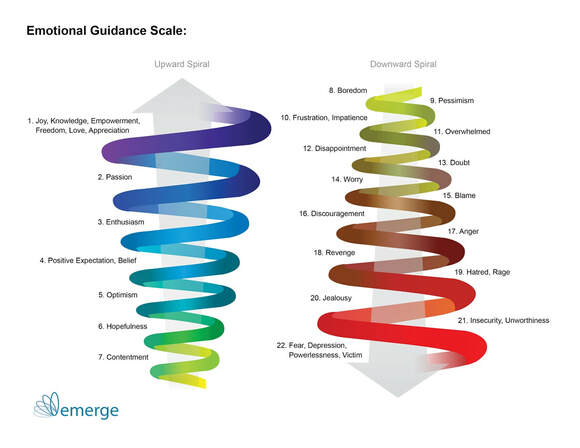
Why does depression happen to some people and not others? Many factors create a predisposition toward depression, though genetics are known to have a prominent role in the cycle. Researchers have isolated genes that make individuals more vulnerable to stress and low moods and affect response to medication. When the inherited vulnerability meets with a psychological or medical injury—an illness, traumatic life event, or persistent stress—the perfect storm for triggering this disorder, individuals may find themselves overwhelmed and unable to withstand the pull into the spiral of negative emotions that ultimately lead to depression. (see image below) Growing up with parental depression or other mental disorders also increases our predisposition to depression and informs our coping skills. We watched and internalized how our parents handled stress and adversity and without intervention are likely to employ the same inadequate responses. One thing is indisputable: succumbing to depression is not a sign of weak character. In fact, men who struggle with debilitating depression may have been better off if they’d sought help sooner. Is it Depression or is it boredom? Many Americans don’t necessarily feel depressed or anxious, but they do feel a tremendous amount of stress, a lack of fulfillment, or constant boredom. A recent study by York University in Toronto defined boredom as the state of an unengaged mind, not connected with the environment or the present moment in a meaningful way. Boredom is marked by a lack of fulfilled desire or satisfying activity. One longitudinal study found that people who reported high levels of boredom were more likely to make performance errors, were less productive, had higher rates of compulsive or risky behaviors such as substance abuse or overeating. These indicators were especially prevalent in men. Boredom is not the same as depression, but it can be the beginning of a downward spiral toward it, as illustrated by the image below. That’s because negative coping responses to boredom create stress, which begets more negative emotions and therefore more stress. Stress is not always a bad thing, actually. The good stress, or Eustress, is the positive stimulus of excitement and anticipation, often prompted by life events such as weddings, births, job promotions, or other milestone events. Eustress allows us to escape the monotony of everyday life and nudges us into the upward spiral towards empowerment and positive emotions. In contrast, Distress negatively affects our mood, behaviors, and relationships, as well as causes physical and cognitive changes. Acute stress puts us into a fight-or-flight mode, while chronic stress keeps us there. The biological response to stress includes elevated heart rate and blood pressure, compromised immune system, impaired memory, and increased likelihood of anxiety and depression. Our bodies begin to break down under the strain of Distress and our minds follow. Recognizing depression is an important step, but it is the first rather than the only step in getting better. Depression impairs a person's ability to think, sleep, get motivated and energized, and evaluate and respond to stressors and life experiences and it has been shown to have biological underpinnings. While the neuroscience of depression is complex (below is a short video with an overview), one thing is undeniable: we cannot simply will ourselves to get better. Healing from depression requires that we make some changes and perhaps seek outside help. What to do in a crisis? We cover the solution in Part II of this blog, but if you or someone you care about is in crisis and at risk of suicide, here is how you can access help: • Call your doctor or therapist • Call 911 or go to the nearest emergency room • Call 24-hour National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255); TTY at 1-800-799-4889. Read Part II of this blog: Too strong for his own good: depression - the silent killer of men. Part II: the solution.
Comments are closed.
|
Categories
All
Archives
March 2023
|
[email protected]



 RSS Feed
RSS Feed